Steroid phobia
Irrational fear of topical steroids can result in under treatment of eczema, resulting in a poor quality of life and poor growth.
Why are topical steroids used to treat eczema?
Steroids occurs naturally in the body and controls inflammation. Topical steroids applied to the skin targets areas where it is needed the most.
What are the dangers of using topical steroids?
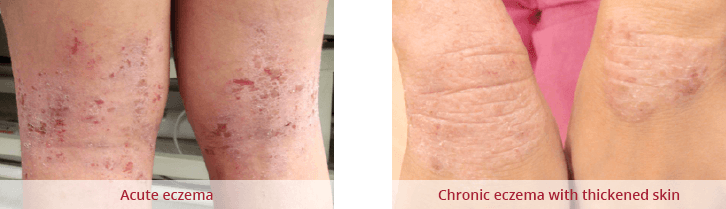
If topical steroids is used in its appropriate strength, quantity, duration and at the correct sites under your doctor’s supervision, skin damage is extremely uncommon. Without using topical steroids, the skin becomes thick, itchy and unsightly. Delayed use of topical steroids leads to worsening of eczema and stronger topical steroids will eventually be required for longer periods of time.
Topical steroid creams should be avoided on eyelid skin though as there is an increased risk of cataracts and glaucoma.
Myths about topical steroids
Topical steroids should not be used on broken or weepy skin: False
The skin is often broken and cracked if you have bad eczema, and topical steroids help to reduce the inflammation. If your skin is very weepy it may be infected, so antibiotics may be needed.
Topical steroids affect growth and development: False
Topical steroids is not the same as anabolic steroids sometimes taken by athletes. They are almost never absorbed into the bloodstream, and so will not affect growth and development or cause other side effects within the body. The body’s ability to fight infections will not be affected. Short courses of steroids may be prescribed for severe eczema flare-ups, but this will not harm the body in the long run.
On the other hand, untreated severe eczema can have a significant effect on physical, psychological and social development, and this can affect children’s growth and development. As the eczema improves with steroid application, the growth and quality of life may improve.
Topical steroids will make me dependent on them: False
There is no evidence that topical steroids cause dependence or addiction.
Topical steroids shouldn’t be needed if I use enough moisturiser: False
Moisturisers only help with the dryness of the skin. Red, itchy or bumpy skin requires topical steroids for effective treatment.
Topical steroids should always be applied in very small amounts: False
Too thin an application results in ineffective treatment. A useful way of knowing the correct amount of topical steroids to apply is to use the fingertip rule.
Alternative and complementary therapies.
Alternative and complementary therapies have not been tried and tested in clinical trials in the same way as topical steroids have. In fact, some may contain steroids in a higher concentration.
The role of food allergy in eczema remains uncertain. Dietary exclusion exclusions should be supervised by doctors as it may affect growth and development.
Topical Steroids.
|
Potency
|
Name
|
Sites
|
|
Very mild
|
Hydrocortisone 1%
|
Face, neck, flexures, body, limbs
|
|
Desonide 0.5%
|
Face, neck, flexures, body, limbs
|
|
Mild
|
Betamethasone 0.025%
|
Face, neck, flexures, body, limbs
|
|
Moderate
|
Betamethasone 0.05%
|
Body, limbs, avoid face, neck and flexures
|
|
Strong
|
Betamethasone 0.1%
|
Body, limbs, avoid face, neck and flexures
|
|
Fucicort
|
Body, limbs, avoid face, neck and flexures
|
|
Momethasone furoate
|
Body, limbs, avoid neck and flexures
May be used on the face for a short period of time
|