What is Rhinitis
Rhinitis is the condition where there is inflammation and irritation of the mucous membranes of the nose. It can be caused by infection, irritant exposure or allergens. Specifically, Allergic Rhinitis is an inflammation of the nasal mucous membranes caused by exposure to inhaled allergens, such as from dust mite, cockroaches, moulds and animal hair. People who are sensitive to these allergens may then experience one or more of the following symptoms that lasts several weeks and does not seem to go away.
- Blocked nose
- Running nose
- Bouts of sneezing
- Itching in the nose/throat
- Mouth breathing
- Throat clearing cough
- Disturbed sleep
In Singapore, about one in six children suffer from rhinitis all year round. Up to 40% of 12-15 year old children suffer from rhinitis. Rhinitis in adults is around 20%.
- Inhaled allergen
- Nasal symptoms
- Eye symptoms
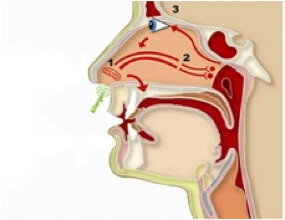
Allergy Rhinitis can sometimes be associated with itchy, watery or puffy eyes (Allergic conjunctivitis).
Non allergic rhinitis with nasal symptoms triggered by the following environmental allergies can also occur.
- Environmental or occupational irritants. Dust, smog, secondhand smoke or strong odors, such as perfumes, can trigger non-allergic rhinitis. Chemical fumes, such as those you might be exposed to in certain occupations, also may be to blame.
- Occupational rhinitis. If you have symptoms of rhinitis are more serious in the work- place, work related rhinitis maybe aggrevated by allergens in the workplace.
- Weather changes. Temperature or humidity changes can trigger the membranes inside your nose to swell and cause a runny or stuffy nose.
- Infections. A common cause of nonallergic rhinitis is a viral infection — a cold.
- Foods and beverages. Non-allergic rhinitis may occur when you eat, especially when eating hot or spicy foods. Drinking alcoholic beverages also may cause the membranes inside your nose to swell, leading to nasal congestion.
- Certain medications. Some medications can cause nonallergic rhinitis. These include aspirin, ibuprofen and high blood pressure (hypertension) medications, such as beta blockers.
- Hormone changes. Hormonal changes due to pregnancy, menstruation, oral contraceptive use or other hormonal conditions such as hypothyroidism.
